Get a plan made for your unique body and goals
Understanding the Difference: Low-FODMAP Diet vs. High-FODMAP Eating

FODMAPs are a group of short-chain carbohydrates (sugars) that aren’t properly absorbed in the gut and trigger symptoms in people with IBS. A low-FODMAP diet can minimize these symptoms by replacing foods that trigger them.
Let’s see how a low vs. high-FODMAP diet impacts the gut, how they differ in their food options, and when it’s actually okay to enjoy (high) FODMAPs.
How the Low-FODMAP Diet Works
According to a narrative review on PubMed, FODMAP stands for all foods that contain fermentable oligosaccharides (soluble plant fibers/prebiotics), disaccharides (lactose/sugar in dairy), monosaccharides (fructose/sugar in fruits), and polyols (sugar alcohols, used as artificial sweeteners and found in some fruits).
They are poorly absorbed in the small intestine and cause bloating, gas, cramping, diarrhea, and constipation. A low-FODMAP diet reduces these symptoms by:
- Easing bloating and pressure: These carbohydrates ferment quickly, producing gas. Reducing them means less gas buildup and bloating.
- Reducing the water in the intestines: FODMAPs draw water into the gut. Limiting them helps prevent intestinal swelling and diarrhea.
- Preventing gut stretches: Less gas and water in the gut means less stretching of the intestinal wall, which reduces pain, gas, and irregular bowel habits.
- Making bowel habits more stable. This diet also improves stool consistency and frequency, whether the main issue is diarrhea, constipation, or both.
High-FODMAP Eating: What Happens in the Gut?
High-FODMAPs aren’t fully digested in the small intestine. As a result, they increase fermentation in the colon and produce gases like hydrogen and methane; they raise osmotic activity in the gut, meaning that they pull extra water into the intestinal lumen and expand it; and amplify symptoms in people with IBS.
It’s important to note that these foods aren’t unhealthy or harmful. Many high-FODMAP foods are nutritious and well-tolerated. However, they do cause symptoms in sensitive individuals due to differences in digestion, gut sensitivity, and motility.
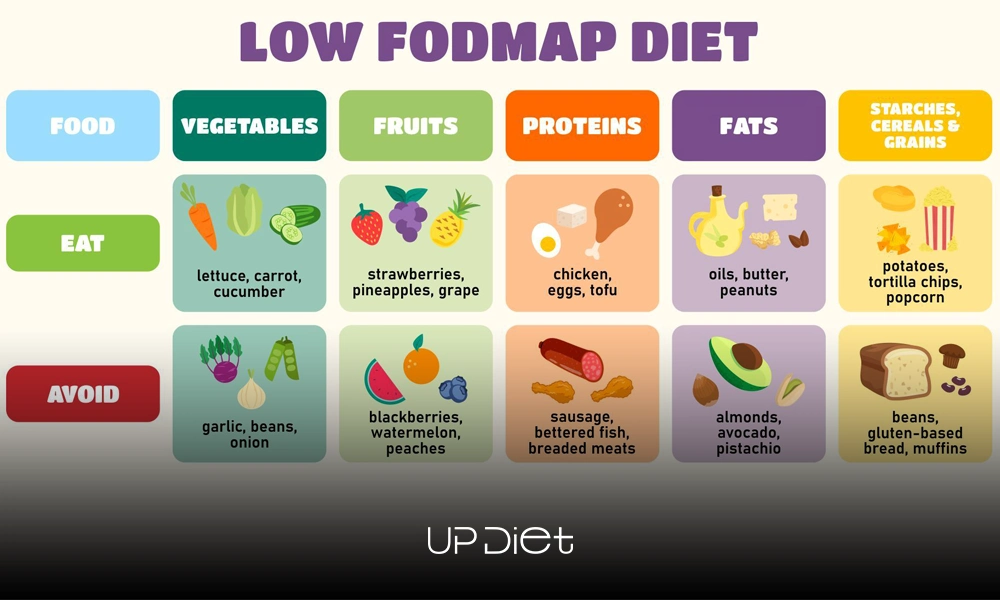
Low-FODMAP vs High-FODMAP: Food Comparison Table
Let’s take a look at low vs. high-FODMAP diet food across different categories. Then we’ll explain how to use them as a symptom-management tool, not as a tool for judging food quality.
Important notes:
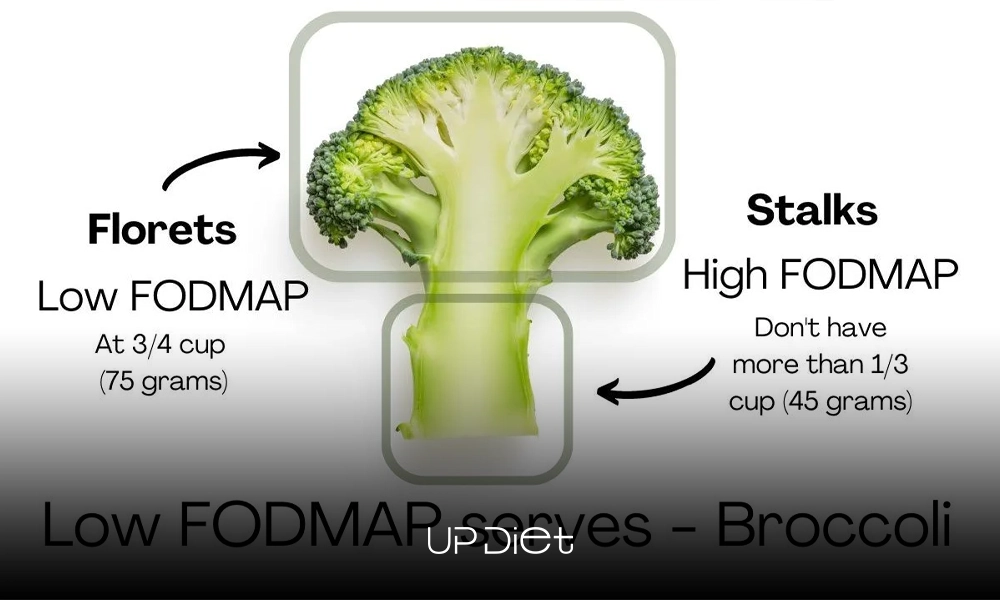
- Serving size is everything when it comes to high-FODMAP diets and foods; something may be low-FODMAP at one serving size but high-FODMAP at a larger one (like almonds, for instance). Plus, FODMAP tolerance is dose-dependent.
- Low-FODMAP doesn’t mean eating without limits. They can still cause symptoms if consumed in excess. Combining several moderate-FODMAPs in one meal can also stack FODMAP load and aggravate symptoms.
- Watch for hidden high-FODMAP ingredients (typically) in sauces, dressings, marinades, sugar-free products, protein bars, flavored yogurts, processed meats, garlic/onion powders, and wheat-based thickeners.
- Studies use low-FODMAP diets for short-term use, followed by planned reintroduction to identify triggers. Long-term restriction of high-FODMAPs isn’t recommended, as it can affect microbiome diversity.
When Is a High-FODMAP Food Actually Okay?
High-FODMAP foods are okay when the portion is below your personal tolerance level, like a slice of bread, a quarter of an apple, or garlic-infused oil. Tolerance also depends on timing and food combinations. When you avoid stacking high-FODMAP foods in the same meal, symptoms are less likely to occur.
Finally, you can enjoy high-FODMAP foods after the reintroduction phase, once your specific triggers and limits are identified.
Final Thoughts
Learning about low- and high-FODMAPs allows you to know which foods (and in what amounts) work for your body to improve digestive comfort. For a tailored approach, consider using tools like UP-Diet, which create personalized low-FODMAP eating plans tailored to your unique triggers and tolerance levels.
- In this post:
- How the Low-FODMAP Diet Works
- High-FODMAP Eating: What Happens in the Gut?
- Low-FODMAP vs High-FODMAP: Food Comparison Table
- When Is a High-FODMAP Food Actually Okay?
- Final Thoughts



